Understanding Retained Placenta: Signs, Treatment, and Recovery
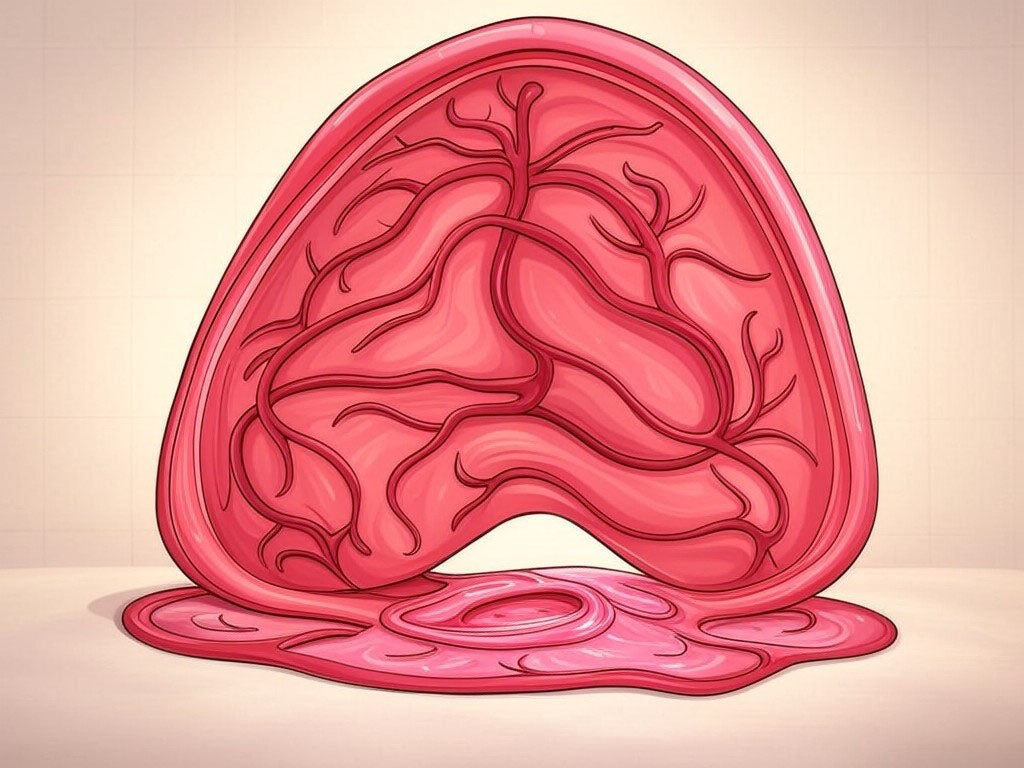
After the joy of welcoming a new baby into the world, the last thing any new mother wants to deal with is complications. One such complication is a retained placenta, a condition where all or part of the placenta stays in the uterus after childbirth. Here's a comprehensive look at this condition:
Signs and Symptoms of Retained Placenta
-
Heavy Postpartum Bleeding: This is the most common symptom. If you're saturating more than four maxi pads in two hours or passing large blood clots, it might indicate a retained placenta.
-
Uterine Pain or Cramping: Continued or intensified pain in the lower abdomen can be a sign that the placenta hasn't fully delivered.
-
Uterine Tenderness: The uterus might feel tender when touched.
-
Fever: A fever could indicate an infection, which can accompany retained placenta.
-
Foul-Smelling Vaginal Discharge: This suggests infection due to retained tissue.
-
Delayed or Absent Placenta Delivery: If the placenta hasn't been delivered within 30-60 minutes after birth, or if you've chosen active management and it hasn't come out within 30 minutes, this is a sign.
When to Seek Medical Attention
You should go in to get checked if:
-
You notice any of the above symptoms.
-
You experience any unusual or severe symptoms post-delivery.
-
There's no sign of the placenta being delivered shortly after your baby.
Procedures for Treating Retained Placenta
Immediate Postpartum:
-
Manual Removal: If the placenta or parts of it are accessible, a healthcare provider might manually remove it using their hand, often under anesthesia or analgesia. This is typically done in the delivery room.
-
Medications: Drugs like oxytocin can be administered to encourage uterine contractions, which might help expel the placenta. Misoprostol might also be used for its ability to contract the uterus.
-
Controlled Cord Traction: If part of the placenta is visible, gentle traction on the umbilical cord might be attempted to deliver the placenta.
If Retained Later:
-
Ultrasound: To confirm if there's retained tissue.
-
Dilation and Curettage (D&C): If manual removal isn't effective or if pieces remain, a D&C might be necessary. This involves dilating the cervix and scraping or using suction to remove any remaining placental tissue.
-
Hysteroscopy: In cases where D&C isn't sufficient or if there's a possibility of deeply embedded tissue, a hysteroscopy uses a camera to guide the removal of the placenta.
Recovery from Retained Placenta
-
Physical Recovery: After treatment, you might experience cramping and bleeding as your body heals. The recovery period can vary but usually spans a few weeks. Pain management and monitoring for signs of infection are key.
-
Monitoring: Regular check-ups post-treatment are necessary to ensure all placental tissue has been removed and there's no infection. Watch for signs like continued heavy bleeding, fever, or severe pain.
-
Emotional Recovery: The experience can be emotionally taxing. Support from healthcare providers, family, or support groups can be invaluable.
Preventive Measures After Birth
-
Active Management of Third Stage: This includes giving an oxytocin injection to help the uterus contract, followed by controlled cord traction to deliver the placenta. This protocol is known to reduce the incidence of retained placenta.
-
Thorough Examination: Post-delivery, the healthcare provider will check the placenta to ensure it's complete. If there's any doubt, further examination or imaging might be done.
-
Breastfeeding: It can help the uterus contract and might aid in expelling any remaining placenta.
-
Vigilance: New mothers should be aware of their body's signals. If something feels off or if bleeding doesn't seem to decrease, speaking up is crucial.
-
Postpartum Ultrasound: In high-risk cases or if there's history, an ultrasound can be performed to check if the uterus is clear.
Retained placenta is a manageable condition when detected early. Understanding the signs, seeking timely medical intervention, and following through with recovery protocols can ensure a safe and healthy postpartum period. As always, open communication with your healthcare provider is vital for your health and well-being after childbirth.
XXX Jessie
Disclaimer: Jessie is not a medical expert; always consult with healthcare professionals for advice specific to your situation. Remember, the information here is for educational purposes and does not replace professional medical advice. Do not share your personally identifiable information.

Dejar un comentario
Este sitio está protegido por hCaptcha y se aplican la Política de privacidad de hCaptcha y los Términos del servicio.